- Home
- Our Clinic
Pain Relief :
Sensivity of Teeth
- Signs & Symptoms
- What causes sensitive teeth?
Tooth sensitivity also known as dentin hypersensitivity - affects the tooth or exposed root surfaces. This occurs when the enamel that protects our teeth gets thinner, or when gum recession occurs, exposing the underlying surface, the dentin, thus, reducing the protection the enamel and gums provide to the tooth and root. Tooth sensitivity affects up to 57% of the population.
If hot, cold, sweet or very acidic foods and drinks, or breathing in cold air, makes your teeth or a tooth sensitive or painful then you may have sensitive teeth. Tooth sensitivity can come and go over time.
The part of the tooth we can see has a layer of enamel that protects the softer dentine underneath. If the dentine is exposed, a tooth can become sensitive. This usually happens where the tooth and the gum meet and the enamel layer is much thinner. Here are some causes of sensitivity:
1. Brushing too hard ('toothbrush abrasion'), and brushing from side to side, can cause enamel to be worn away - particularly where the teeth meet the gums. The freshly exposed dentine may then become sensitive.
2. Dental erosion: this is loss of tooth enamel caused by attacks of acid from acidic food and drinks. If enamel is worn away, the dentine underneath is exposed which may lead to sensitivity.
3. Gums may naturally recede (shrink back), and the roots of the teeth will become exposed and can be more sensitive. Root surfaces do not have an enamel layer to protect them.
4. Gum disease: a build-up of plaque or tartar can cause the gum to recede down the tooth and even destroy the bony support of the tooth. Pockets can form in the gums around the tooth, making the area difficult to keep clean and the problem worse.
5. Tooth grinding: this is a habit which involves clenching and grinding the teeth together. This can cause the enamel of the teeth to be worn away, making the teeth sensitive.
6. A cracked tooth or filling: a cracked tooth is one that has become broken. A crack can run from the biting surface of a tooth down towards the root. Extreme temperatures, especially cold, may cause discomfort.
7. Tooth bleaching: some patients have sensitivity for a short time during bleaching or afterwards. Discuss this with your dental team before having treatment.
Type of treatment
1. Desensitizing toothpaste. This contains compounds that help block transmission of sensation from the tooth surface to the nerve, and usually requires several applications before the sensitivity is reduced
2. Fluoride gel. An in-office technique which strengthens tooth enamel and reduces the transmission of sensations.
3. A crown, inlay or bonding. These may be used to correct a flaw or decay that results in sensitivity.
4. Surgical gum graft. If gum tissue has been lost from the root, this will protect the root and reduce sensitivity.
5. Root canal. If sensitivity is severe and persistent and cannot be treated by other means, your dentist may recommend this treatment to eliminate the problem.
Routine Dental Care
- Fillings: in initial stages of cavities
- Root canals: for tooth having infected pulp tissues
- Non-routine x-rays
- Periodontal scaling: During a cleaning, tartar is removed from the patient's teeth, and that helps to prevent tooth decay. The removal of tartar also improves gum health and the appearance of the person's teeth.
- • Root planning: removal of infected surface on root surface to restore gums health.
Dental care is the maintenance of healthy teeth and may refer to: Oral hygiene, the practice of keeping the mouth and teeth clean in order to prevent dental disorders.
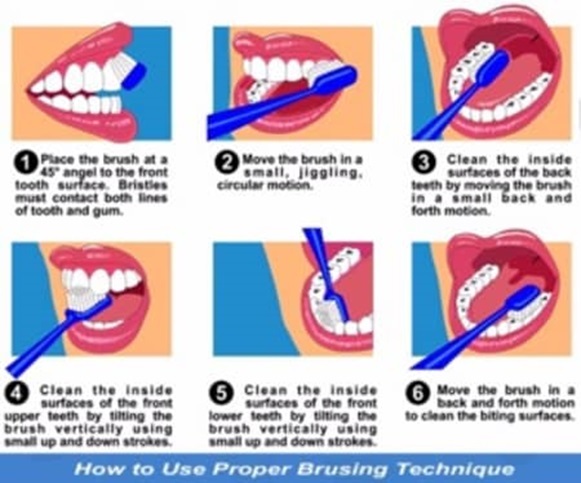
Brush your teeth at least twice a day (morning and before bed time)
Floss at least once a day.
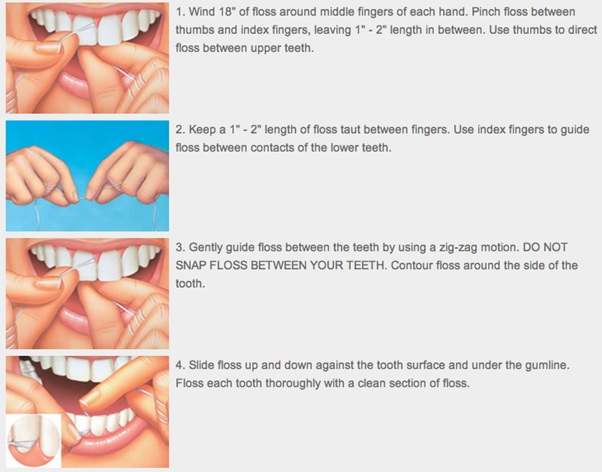
These activities remove plaque, which if not removed, combines with sugars to form acids that lead to tooth decay.
Regular check up
Routine dental check up twice a year is an essential part of keeping teeth and gums healthy
It includes primary check-up for cavities, tartar (calculus), gum problems in earlier stage, mal-aligned teeth in growing kids, etc...
The basic services include common dental treatments like fillings and root canals.
Root Canal Therapy
- A cracked tooth
- Cosmetic Procedure
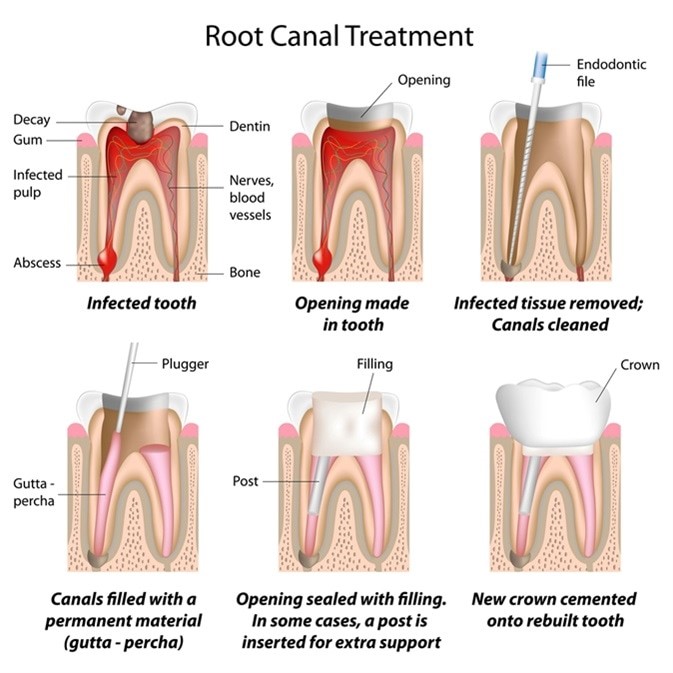
Root Canal Treatment (RCT) is the removal of the tooth's pulp, a small, thread-like tissue in the centre of the tooth. Once the damaged, diseased or dead pulp is removed, the remaining space is cleaned, shaped and filled. This procedure seals off the root canal. Years ago, teeth with diseased or injured pulps were removed. Today, root canal treatment saves many teeth that would otherwise be lost.
The most common causes of pulp damage or death are:
An injury to a tooth, such as a severe knock to the tooth, either recent or in the past.
Once the pulp is infected or dead, if left untreated, pus can build up at the root tip in the jawbone, forming an abscess. An abscess can destroy the bone surrounding the tooth and cause pain.
How long will the Restored Tooth Last?
Your treated and restored tooth/teeth can last a lifetime with proper care. Because tooth decay can still occur in treated teeth, good oral hygiene and regular dental exams are necessary to prevent further problems.
As there is no longer a pulp keeping the tooth alive, root-treated teeth can become brittle and are more prone to fracture. This is an important consideration when deciding whether to crown or fill a tooth after root canal treatment.
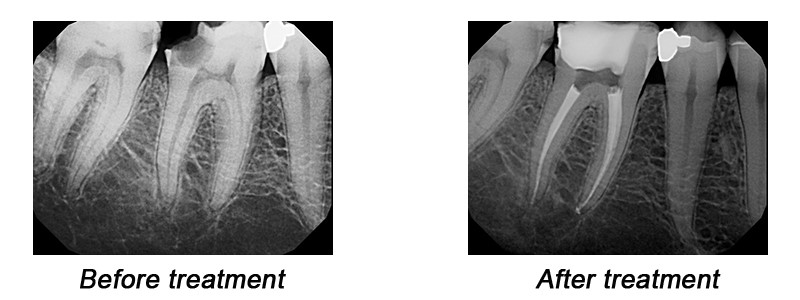
To determine the success or failure of root canal treatment, the most relied-upon method is to compare new X-rays with those taken prior to treatment. This comparison will show whether bone continues to be lost or is being regenerated.
Steps of Root Canal Treatment
Retreatment of failed Root Canal
Root canal treatment is a procedure with a high success rate of more than 95%. Unfortunately, in a 5% of cases root canal complications result in a failed root canal. The success of root canal therapy depends on a number of different factors and the likelihood of failure can vary considerably from case to case.
However, some of the root canal complications are not predictable.
There are three options available after a failed root canal
1. The first option for solving the problems of a failed root canal is the root canal re-treatment.
2. Depending on the nature of the problem, the doctor may decide that endodontic surgery must be performed in order to save the tooth. The procedure is called apicoectomy and it involves the surgical removal of the root's tip (apex). A small filling (retro fill) is then used to seal the root.
3. The chances for a successful treatment of a failed root canal are between 50% and 75%. In some cases, despite root canal retreatment or endodontic surgery, tooth extraction must be performed. The lost tooth is recommended to be replaced as soon as possible to prevent more teeth problems The best solution for tooth replacement after extraction is to replace the lost tooth with a dental implant.
At Shah multi-speciality Dental Clinic, we have expertise for the retreatment of failed procedures.
Wisdom Teeth Removal
Disimpaction of Wisdom Molars :
The most common impactions are seen in cases of wisdom teeth (third molars). Sometimes, even canines or other teeth might be found impacted in one's mouth.
Each individual wisdom tooth is unique and depending on how it grows, it can have different impact on bones and/or tissues. Their varied developments may affect other teeth and cause troubles. When they need to be removed, experts from Shah Dental Clinic are the ones who can easily help you.
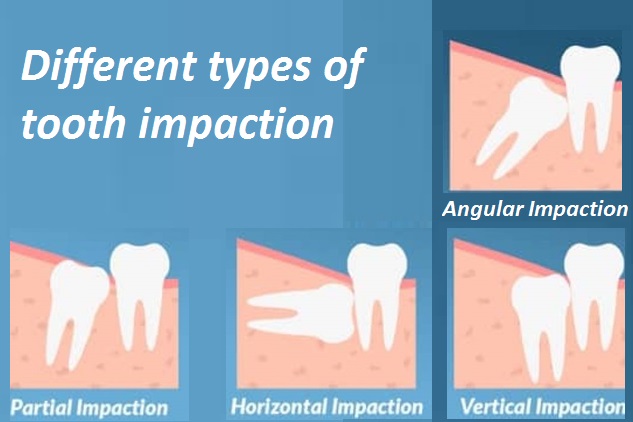
If the impaction is between the third molar and part of the second molar, this kind is called bone impaction. It can sub categorized into vertical, horizontal, and angular depending on the way they are intersecting. If the wisdom tooth is directly breaking out of the tissue, it is known as tissue impaction.
The following four impactions are commonly found in patients :
Bone Impaction (Vertical) :Impaction would cause pathosis inside the cheek bone or jaw bone.
Bone Impaction (Horizontal) :Besides leading pathosis, horizontal placement would hurt the hard tissue of the second molar to cause toothache and cavities.
Bone Impaction (Angular) :Besides leading pathosis, angular placement would hurt the hard tissue of the second molar to cause toothache and cavities.
Tissue Impaction :The wisdom tooth almost erupts out of gum, or its half erupts out of gum to cause pseudo-pocket. Besides leading pathosis, it easily tracts food debris and causes gum irritation.

Jaw Pain (TMJ Disorder)
Have you ever experienced ‘clicking’ sound while opening/closing your jaw or does your jaw deviate to right/left side during jaw movements? If yes, you might be having TMJ problem.
What is a TMJ disorder? How does it happen?
TMJ (Temporomandibular Joint) disorders are related to your complex jaw joint. TMJ disorders develop for many reasons. It might be due to excessive clenching or grinding of your teeth, tightening your jaw muscles and stressing your TM joint or, a damaged jaw joint due to injury or disease.
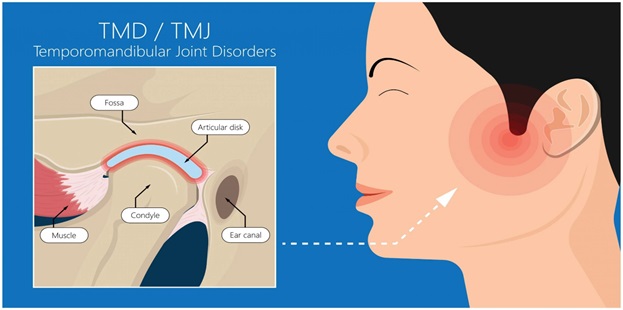
Whatever the cause, it causes misaligned bite, pain, clicking sound while mouth opening or trouble in opening your mouth wide.
Some types of TMJ problems can lead to highly painful conditions if left untreated for a long time. So, it is always suggested that you visit your dentist as soon as you feel any pain or discomfort so that the treatment can be started early and you are completely cured.
Nowadays, these problems are much easily diagnosed than it used to be earlier. With the advancements of dentistry, any dental problem has become so easily diagnosable and treatable. You just have to visit your dentist at the earliest and you will be cured.
What are the treatment options for a TMJ problem?
There are various treatment options that can help to improve the harmony and function of your jaw. It depends on the condition you have.
It is important to note that the treatment always works best with a team approach of self-care as well as professional care. So, even after it has been cured, you have to maintain it the way you are instructed.
